Quest for the right Drug
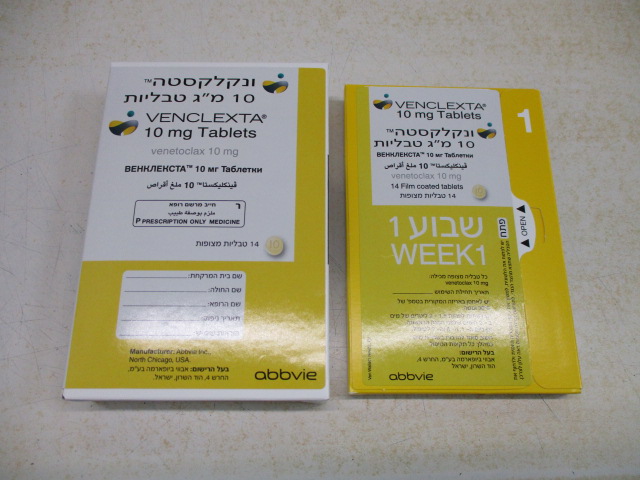
ונקלקסטה 10 מ"ג טבליות VENCLEXTA 10 MG TABLETS (VENETOCLAX)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
6 ADVERSE REACTIONS The following clinically significant adverse reactions are described elsewhere in the labeling: • Tumor Lysis Syndrome [see Warnings and Precautions (5.1)] • Neutropenia [see Warnings and Precautions (5.2)] • Infections [see Warnings and Precautions (5.3)] 6.1 Clinical Trials Experience Because clinical trials are conducted under widely variable conditions, adverse event rates observed in clinical trials of a drug cannot be directly compared with rates of clinical trials of another drug and may not reflect the rates observed in practice. In CLL/SLL, the safety population reflects exposure to VENCLEXTA as monotherapy in patients in M13-982, M14-032, and M12-175 and in combination with obinutuzumab or rituximab in patients in CLL14 and MURANO. In this CLL/SLL safety population, the most common adverse reactions (≥20%) for VENCLEXTA were neutropenia, thrombocytopenia, anemia, diarrhea, nausea, upper respiratory tract infection, cough, musculoskeletal pain, fatigue, and edema. In AML, the safety population reflects exposure to VENCLEXTA in combination with decitabine, azacitidine, or low-dose cytarabine in patients in M14-358, VIALE-A, and VIALE- C. In this safety population, the most common adverse reactions (≥30% in any trial) were nausea, diarrhea, thrombocytopenia, constipation, neutropenia, febrile neutropenia, fatigue, vomiting, edema, pyrexia, pneumonia, dyspnea, hemorrhage, anemia, rash, abdominal pain, sepsis, musculoskeletal pain, dizziness, cough, oropharyngeal pain, and hypotension. Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma VENCLEXTA in Combination with Obinutuzumab The safety of VENCLEXTA in combination with obinutuzumab (VEN+G) (N=212) versus obinutuzumab in combination with chlorambucil (GClb) (N=214) was evaluated in CLL14, a randomized, open-label, actively controlled trial in patients with previously untreated CLL [see Clinical Studies (14.1)]. Patients randomized to the VEN+G arm were treated with VENCLEXTA and obinutuzumab in combination for six cycles, then with VENCLEXTA as monotherapy for an additional six cycles. Patients initiated the first dose of the 5-week ramp-up for VENCLEXTA on Day 22 of Cycle 1 and once completed, continued VENCLEXTA 400 mg orally once daily for a total of 12 cycles. The trial required a total Cumulative Illness Rating Scale (CIRS) >6 or CLcr <70 mL/min, hepatic transaminases and total bilirubin ≤2 times upper limit of normal and excluded patients with any individual organ/system impairment score of 4 by CIRS except eye, ear, nose, and throat organ system. The median duration of exposure to VENCLEXTA was 10.5 months (range: 0 to 13.5 months) and the median number of cycles of obinutuzumab was 6 in the VEN+G arm. Serious adverse reactions were reported in 49% of patients in the VEN+G arm, most often due to febrile neutropenia and pneumonia (5% each). Fatal adverse reactions that occurred in the absence of disease progression and with onset within 28 days of the last study treatment were reported in 2% (4/212) of patients, most often from infection. In the VEN+G arm, adverse reactions led to treatment discontinuation in 16% of patients, dose reduction in 21%, and dose interruption in 74%. Neutropenia led to discontinuation of VENCLEXTA in 2% of patients, dose reduction in 13%, and dose interruption in 41%. Table 9 presents adverse reactions identified in CLL14. Table 9. Adverse Reactions (≥10%) in Patients Treated with VEN+G in CLL14 VENCLEXTA + Obinutuzumab Obinutuzumab + Chlorambucil (N = 212) (N = 214) Adverse Reaction All Grades Grade ≥ 3 All Grades Grade ≥ 3 (%) (%) (%) (%) Blood and lymphatic system disorders Neutropeniaa 60 56 62 52 a Anemia 17 8 20 7 Gastrointestinal disorders Diarrhea 28 4 15 1 Nausea 19 0 22 1 Constipation 13 0 9 0 Vomiting 10 1 8 1 General disorders and administration site conditions Fatiguea 21 2 23 1 Infections and infestations Upper respiratory 17 1 17 1 tract infectiona a Includes multiple adverse reaction terms. Other clinically important adverse reactions (All Grades) reported in <10% of patients treated with VEN+G are presented below: Blood and lymphatic system disorders: febrile neutropenia (6%) Infection and infestations (all include multiple adverse reaction terms): pneumonia (9%), urinary tract infection (6%), sepsis (4%) Metabolism and nutrition disorder: tumor lysis syndrome (1%) During treatment with VENCLEXTA monotherapy after completion of VEN+G, the adverse reaction that occurred in ≥10% of patients was neutropenia (26%). The grade ≥3 adverse reactions that occurred in ≥2% of patients were neutropenia (23%) and anemia (2%). Table 10 presents laboratory abnormalities CLL14. Table 10. New or Worsening Clinically Important Laboratory Abnormalities (≥10%) in Patients Treated with VEN+G in CLL14 VENCLEXTA + Obinutuzumab + Obinutuzumab Chlorambucil (N = 212) (N = 214) Laboratory Abnormalitya All Grades Grade 3 or 4 All Grades Grade 3 or 4 (%) (%) (%) (%) Hematology Leukopenia 90 46 89 41 Lymphopenia 87 57 87 51 Neutropenia 83 63 79 56 Thrombocytopenia 68 28 71 26 Anemia 53 15 46 11 Chemistry Blood creatinine increased 80 6 74 2 Hypocalcemia 67 9 58 4 Hyperkalemia 41 4 35 3 Hyperuricemia 38 38 38 38 a Includes laboratory abnormalities that were new or worsening, or with worsening from baseline unknown. Grade 4 laboratory abnormalities that developed in ≥2% of patients treated with VEN+G included neutropenia (32%), leukopenia and lymphopenia (10%), thrombocytopenia (8%), hypocalcemia (8%), hyperuricemia (7%), blood creatinine increased (3%), hypercalcemia (3%), and hypokalemia (2%). VENCLEXTA in Combination with Rituximab The safety of VENCLEXTA in combination with rituximab (VEN+R) (N=194) versus bendamustine in combination with rituximab (B+R) (N=188) was evaluated in MURANO [see Clinical Studies (14.1)]. Patients randomized to VEN+R completed the scheduled ramp-up (5 weeks) and received VENCLEXTA 400 mg once daily, in combination with rituximab for 6 cycles followed by VENCLEXTA monotherapy, for a total of 24 months after ramp-up. At the time of analysis, the median duration of exposure to VENCLEXTA was 22 months and the median number of cycles of rituximab was 6 in the VEN+R arm. Serious adverse reactions were reported in 46% of patients in the VEN+R arm, with most frequent (≥5%) being pneumonia (9%). Fatal adverse reactions that occurred in the absence of disease progression and within 30 days of the last VENCLEXTA treatment and/or 90 days of last rituximab were reported in 2% (4/194) of patients. In the VEN+R arm, adverse reactions led to treatment discontinuation in 16% of patients, dose reduction in 15%, and dose interruption in 71%. Neutropenia and thrombocytopenia each led to discontinuation of VENCLEXTA in 3% of patients. Neutropenia led to dose interruption of VENCLEXTA in 46% of patients. Table 11 presents adverse reactions identified in MURANO. Table 11. Adverse Reactions (≥10%) in Patients Treated with VEN+R in MURANO VENCLEXTA + Rituximab Bendamustine + Rituximab (N = 194) (N = 188) Adverse Reaction All Grades Grade ≥ 3 All Grades Grade ≥ 3 (%) (%) (%) (%) Blood and lymphatic system disorders Neutropeniaa 65 62 50 44 a Anemia 16 11 23 14 Gastrointestinal disorders Diarrhea 40 3 17 1 Nausea 21 1 34 1 Constipation 14 <1 21 0 Infections and infestations Upper respiratory 39 2 23 2 tract infectiona Lower respiratory 18 2 10 2 tract infectiona Pneumoniaa 10 7 14 10 General disorders and administration site conditions Fatiguea 22 2 26 <1 a Includes multiple adverse reaction terms. Other clinically important adverse reactions (All Grades) reported in <10% of patients treated with VEN+R are presented below: Blood and lymphatic system disorders: febrile neutropenia (4%) Gastrointestinal disorders: vomiting (8%) Infections and infestations: sepsis (<1%) Metabolism and nutrition disorders: tumor lysis syndrome (3%) During treatment with VENCLEXTA monotherapy after completion of VEN+R combination treatment, adverse reactions that occurred in ≥10% of patients were upper respiratory tract infection (21%), diarrhea (19%), neutropenia (16%), and lower respiratory tract infections (11%). The Grade 3 or 4 adverse reactions that occurred in ≥2% of patients were neutropenia (12%) and anemia (3%). Table 12 presents laboratory abnormalities identified in MURANO. Table 12. New or Worsening Clinically Important Laboratory Abnormalities (≥10%) in Patients Treated with VEN+R in MURANO VENCLEXTA + Rituximab Bendamustine + Rituximab (N = 194) (N = 188) Laboratory Abnormality All Grades a Grade 3 or 4 All Gradesa Grade 3 or 4 (%) (%) (%) (%) Hematology Leukopenia 89 46 81 35 Lymphopenia 87 56 79 55 Neutropenia 86 64 84 59 Anemia 50 12 63 15 Thrombocytopenia 49 15 60 20 Chemistry Blood creatinine increased 77 <1 78 1 Hypocalcemia 62 5 51 2 Hyperuricemia 36 36 33 33 Hyperkalemia 24 3 19 2 a Includes laboratory abnormalities that were new or worsening, or with worsening from baseline unknown. Grade 4 laboratory abnormalities that developed in ≥2% of patients treated with VEN+R included neutropenia (31%), lymphopenia (16%), leukopenia (6%), thrombocytopenia (6%), hyperuricemia (4%), hypocalcemia (2%), hypoglycemia (2%), and hypermagnesemia (2%). VENCLEXTA as Monotherapy The safety of VENCLEXTA was evaluated in pooled data from three single-arm trials (M13- 982, M14-032, and M12-175). Patients received VENCLEXTA 400 mg orally once daily after completing the ramp-up phase (N= 352). The median duration of treatment with VENCLEXTA at the time of data analysis was 14.5 months (range: 0 to 50 months). Fifty-two percent of patients received VENCLEXTA for more than 60 weeks. In the pooled dataset, the median age was 66 years (range: 28 to 85 years), 93% were White, and 68% were male. The median number of prior therapies was 3 (range: 0 to 15). Serious adverse reactions were reported in 52% of patients, with the most frequent (≥5%) being pneumonia (9%), febrile neutropenia (5%), and sepsis (5%). Fatal adverse reactions that occurred in the absence of disease progression and within 30 days of venetoclax treatment were reported in 2% of patients in the VENCLEXTA monotherapy studies, most often (2 patients) from septic shock. Adverse reactions led to treatment discontinuation in 9% of patients, dose reduction in 13%, and dose interruption in 36%. The most frequent adverse reactions leading to drug discontinuation were thrombocytopenia and autoimmune hemolytic anemia. The most frequent adverse reaction (≥5%) leading to dose reductions or interruptions was neutropenia (8%). Table 13 presents adverse reactions identified in these trials. Table 13. Adverse Reactions Reported in ≥10% (All Grades) or ≥5% (Grade ≥3) of Patients with Previously Treated CLL/SLL Who Received VENCLEXTA Monotherapy VENCLEXTA (N = 352) Adverse Reaction All Grades Grade ≥3 (%) (%) Blood and lymphatic system disorders Neutropeniaa 50 45 a Anemia 33 18 a Thrombocytopenia 29 20 a Lymphopenia 11 7 Febrile neutropenia 6 6 Gastrointestinal disorders Diarrhea 43 3 Nausea 42 1 a Abdominal pain 18 3 Vomiting 16 1 Constipation 16 <1 a Mucositis 13 <1 Infections and infestations Upper respiratory tract infectiona 36 1 a Pneumonia 14 8 VENCLEXTA (N = 352) Adverse Reaction All Grades Grade ≥3 (%) (%) a Lower respiratory tract infection 11 2 General disorders and administration site conditions Fatiguea 32 4 a Edema 22 2 Pyrexia 18 <1 Musculoskeletal and connective tissue disorders Musculoskeletal paina 29 2 Arthralgia 12 <1 Respiratory, thoracic, and mediastinal disorders Cougha 22 0 a Dyspnea 13 1 Nervous system disorders Headache 18 <1 a Dizziness 14 0 Skin and subcutaneous tissue disorders Rasha 18 <1 Adverse reactions graded using NCI Common Terminology Criteria for Adverse Events version 4.0. a Includes multiple adverse reaction terms. Table 14 presents laboratory abnormalities reported throughout treatment that were new or worsening from baseline. The most common (>5%) Grade 4 laboratory abnormalities observed with VENCLEXTA monotherapy were hematologic laboratory abnormalities, including neutropenia (33%), leukopenia (11%), thrombocytopenia (15%), and lymphopenia (9%). Table 14. New or Worsening Laboratory Abnormalities in ≥40% (All Grades) or ≥10% (Grade 3 or 4) of Patients with Previously Treated CLL/SLL Who Received VENCLEXTA Monotherapy VENCLEXTA (N = 352) Laboratory Abnormality a All Grades Grade 3 or 4 (%) (%) Hematology Leukopenia 89 42 Neutropenia 87 63 Lymphopenia 74 40 Anemia 71 26 Thrombocytopenia 64 31 Chemistry VENCLEXTA (N = 352) Laboratory Abnormality All Gradesa Grade 3 or 4 (%) (%) Hypocalcemia 87 12 Hyperglycemia 67 7 Hyperkalemia 59 5 AST increased 53 3 Hypoalbuminemia 49 2 Hypophosphatemia 45 11 Hyponatremia 40 9 a Includes laboratory abnormalities that were new or worsening, or worsening from baseline unknown. Important Adverse Reactions in CLL/SLL Tumor Lysis Syndrome Tumor lysis syndrome is an important identified risk when initiating VENCLEXTA. CLL14 The incidence of TLS was 1% (3/212) in patients treated with VEN+G [see Warnings and Precautions (5.1)]. All three events of TLS resolved and did not lead to withdrawal from the trial. Obinutuzumab administration was delayed in two cases in response to the TLS events. MURANO The incidence of TLS was 3% (6/194) in patients treated with VEN+R. After 77/389 patients were enrolled in the trial, the protocol was amended to incorporate the current TLS prophylaxis and monitoring measures described in sections 2.2 and 2.4 [see Dosage and Administration (2.2, 2.4)]. All events of TLS occurred during the VENCLEXTA ramp-up period and were resolved within two days. All six patients completed the ramp-up and reached the recommended daily dose of 400 mg of VENCLEXTA. No clinical TLS was observed in patients who followed the current 5-week ramp-up schedule and TLS prophylaxis and monitoring measures [see Dosage and Administration (2.2, 2.4)]. Rates of laboratory abnormalities relevant to TLS for patients treated with VEN+R are presented in Table 12. Monotherapy Studies (M13-982 and M14-032) In 168 patients with CLL treated according to recommendations described in sections 2.1 and 2.2, the rate of TLS was 2% [see Dosage and Administration (2.2, 2.4)]. All events either met laboratory TLS criteria (laboratory abnormalities that met ≥2 of the following within 24 hours of each other: potassium >6 mmol/L, uric acid >476 µmol/L, calcium <1.75 mmol/L, or phosphorus >1.5 mmol/L), or were reported as TLS events. The events occurred in patients who had a lymph node(s) ≥5 cm and/or absolute lymphocyte count (ALC) ≥25 x 109/L. All events resolved within 5 days. No TLS with clinical consequences such as acute renal failure, cardiac arrhythmias, or sudden death and/or seizures was observed in these patients. All patients had CLcr ≥50 mL/min. Laboratory abnormalities relevant to TLS were hyperkalemia (17% all Grades, 1% Grade ≥3), hyperphosphatemia (14% all Grades, 2% Grade ≥3), hypocalcemia (16% all Grades, 2% Grade ≥3), and hyperuricemia (10% all Grades, <1% Grade ≥3). In the initial Phase 1 dose-finding trials, which had shorter (2-3 week) ramp-up phase and higher starting doses, the incidence of TLS was 13% (10/77; 5 laboratory TLS, 5 clinical TLS), including 2 fatal events and 3 events of acute renal failure, 1 requiring dialysis. After this experience, TLS risk assessment, dosing regimen, TLS prophylaxis and monitoring measures were revised [see Dosage and Administration (2.2, 2.4)]. Acute Myeloid Leukemia VENCLEXTA in Combination with Azacitidine The safety of VENCLEXTA in combination with azacitidine (VEN+AZA) (N=283) versus placebo in combination with azacitidine (PBO+AZA) (N=144) was evaluated in VIALE-A, a double-blind, randomized trial, in patients with newly diagnosed AML [see Clinical Studies (14.2)]. At baseline, patients were ≥75 years of age or had comorbidities that precluded the use of intensive induction chemotherapy based on at least one of the following criteria: baseline ECOG performance status of 2-3, severe cardiac or pulmonary comorbidity, moderate hepatic impairment, CLcr < 45 mL/min, or other comorbidity. Patients were randomized to receive VENCLEXTA 400 mg orally once daily after completion of the ramp-up phase in combination with azacitidine (75 mg/m2 either intravenously or subcutaneously on Days 1-7 of each 28-day cycle) or placebo in combination with azacitidine. Among patients who received VEN+AZA, the median duration of exposure to VENCLEXTA was 7.6 months (range: <0.1 to 30.7 months). Serious adverse reactions were reported in 83% of patients who received VEN+AZA, with the most frequent (≥5%) being febrile neutropenia (30%), pneumonia (22%), sepsis (excluding fungal; 19%), and hemorrhage (6%). Fatal adverse reactions occurred in 23% of patients who received VEN+AZA, with the most frequent (≥2%) being pneumonia (4%), sepsis (excluding fungal; 3%), and hemorrhage (2%). Adverse reactions led to permanent discontinuation of VENCLEXTA in 24% of patients, dose reductions in 2%, and dose interruptions in 72%. Adverse reactions which led to discontinuation of VENCLEXTA in ≥2% of patients were sepsis (excluding fungal; 3%) and pneumonia (2%). The most frequent adverse reaction leading to dose reduction was pneumonia (0.7%). Adverse reactions which required a dose interruption in ≥5% of patients included febrile neutropenia (20%), neutropenia (20%), pneumonia (14%), sepsis (excluding fungal; 11%), and thrombocytopenia (10%). Among patients who achieved bone marrow clearance of leukemia, 53% underwent dose interruptions for absolute neutrophil count (ANC) <500/microliter. Table 15 presents adverse reactions identified in VIALE-A. Table 15. Adverse Reactions (≥10%) in Patients with AML Who Received VEN+AZA with a Difference Between Arms of ≥5% for All Grades or ≥2% for Grade 3 or 4 Reactions Compared with PBO+AZA in VIALE-A VENCLEXTA + Azacitidine Placebo + Azacitidine (N = 283) (N = 144) Adverse Reaction All Grades Grade 3 or 4 All Grades Grade 3 or 4 (%) (%) (%) (%) Gastrointestinal disorders Nausea 44 2 35 <1 a Diarrhea 43 5 33 3 b Vomiting 30 2 23 <1 c Stomatitis 18 1 13 0 d Abdominal pain 18 <1 13 0 Blood and lymphatic system disorders Febrile neutropenia 42 42 19 19 Musculoskeletal and connective tissue disorders Musculoskeletal paine 36 2 28 1 General disorders and administration site conditions Fatiguef 31 6 23 2 g Edema 27 <1 19 0 Vascular disorders Hemorrhageh 27 7 24 3 i Hypotension 12 5 8 3 Metabolism and nutrition disorders Decreased appetitej 25 4 17 <1 Skin and subcutaneous tissue disorders Rashk 25 1 15 0 Infections and infestations Sepsisl (excluding fungal) 22 22 16 14 m Urinary tract infection 16 6 9 6 Respiratory, thoracic and mediastinal disorders Dyspnean 18 4 10 2 Nervous system disorders Dizzinesso 17 <1 8 <1 a Includes diarrhea and colitis. VENCLEXTA + Azacitidine Placebo + Azacitidine (N = 283) (N = 144) Adverse Reaction All Grades Grade 3 or 4 All Grades Grade 3 or 4 (%) (%) (%) (%) b Includes vomiting and hematemesis. c Includes stomatitis, mouth ulceration, mucosal inflammation, cheilitis, aphthous ulcer, glossitis, and tongue ulceration. d Includes abdominal pain, abdominal pain upper, abdominal discomfort, and abdominal pain lower. e Includes arthralgia, back pain, pain in extremity, musculoskeletal pain, bone pain, myalgia, neck pain, non-cardiac chest pain, arthritis, musculoskeletal chest pain, musculoskeletal stiffness, spinal pain, and musculoskeletal discomfort. f Includes fatigue and asthenia. g Includes edema peripheral, edema, generalized edema, eyelid edema, face edema, penile edema, periorbital edema, and swelling. h Includes epistaxis, hematuria, conjunctival hemorrhage, hemoptysis, hemorrhoidal hemorrhage, gingival bleeding, mouth hemorrhage, hemorrhage intracranial, vaginal hemorrhage, cerebral hemorrhage, gastrointestinal hemorrhage, muscle hemorrhage, skin hemorrhage, upper gastrointestinal hemorrhage, anal hemorrhage, eye hemorrhage, gastritis hemorrhagic, hemorrhage, hemorrhage urinary tract, hemorrhagic diathesis, hemorrhagic stroke, hemorrhagic vasculitis, lower gastrointestinal hemorrhage, mucosal hemorrhage, penile hemorrhage, post procedural hemorrhage, rectal hemorrhage, retinal hemorrhage, shock hemorrhagic, soft tissue hemorrhage, subdural hemorrhage, tongue hemorrhage, urethral hemorrhage, vessel puncture site hemorrhage, vitreous hemorrhage and wound hemorrhage. i Includes hypotension and orthostatic hypotension. j Includes decreased appetite and hypophagia. k Includes rash, rash maculo-papular, rash macular, drug eruption, rash papular, rash pustular, eczema, rash erythematous, rash pruritic, dermatitis acneiform, rash morbilliform, dermatitis, eczema asteatotic, exfoliative rash, and perivascular dermatitis. l Includes sepsis, escherichia bacteremia, escherichia sepsis, septic shock, bacteremia, staphylococcal bacteremia, klebsiella bacteremia, staphylococcal sepsis, streptococcal bacteremia, enterococcal bacteremia, klebsiella sepsis, pseudomonal bacteremia, pseudomonal sepsis, urosepsis, bacterial sepsis, clostridial sepsis, enterococcal sepsis, neutropenic sepsis, and streptococcal sepsis. m Includes urinary tract infection, escherichia urinary tract infection, cystitis, urinary tract infection enterococcal, urinary tract infection bacterial, pyelonephritis acute, and urinary tract infection pseudomonal. n Includes dyspnea, dyspnea exertional, and dyspnea at rest. o Includes dizziness and vertigo. Other clinically important adverse reactions (All Grades) at ≥10% that did not meet criteria for Table 15 or <10% are presented below: Hepatobiliary disorders: cholecystitis/cholelithiasisa (4%) Infections and infestations: pneumoniab (33%) Metabolism and nutrition disorders: tumor lysis syndrome (1%) Nervous system disorders: headachec (11%) Investigations: weight decreased (13%). a Includes cholecystitis acute, cholelithiasis, cholecystitis, and cholecystitis chronic. b Includes pneumonia, lung infection, pneumonia fungal, pneumonia klebsiella, atypical pneumonia, lower respiratory tract infection, pneumonia viral, lower respiratory tract infection fungal, pneumonia hemophilus, pneumonia pneumococcal, and pneumonia respiratory syncytial viral. c Includes headache and tension headache. Table 16 presents laboratory abnormalities identified in VIALE-A. Table 16. New or Worsening Laboratory Abnormalities (≥10%) in Patients with AML Who Received VEN+AZA with a Difference Between Arms of ≥5% for All Grades or ≥ 2% for Grade 3 or 4 Reactions Compared with PBO+AZA in VIALE-A VENCLEXTA + Placebo + Azacitidine Azacitidine Laboratory Abnormality All Grades Grade 3 or 4 All Grades Grade 3 or 4 (%) (%) (%) (%) Hematology Neutrophils decreased 98 98 88 81 Platelet decreased 94 88 94 80 Lymphocytes decreased 91 71 72 39 Hemoglobin decreased 61 57 56 52 Chemistry Bilirubin increased 53 7 40 4 Calcium decreased 51 6 39 9 Sodium decreased 46 14 47 8 Alkaline phosphatase increased 42 1 29 <1 Blood bicarbonate decreased 31 <1 25 0 The denominator used to calculate the rate varied from 85 to 144 in the PBO+AZA arm and from 125 to 283 in the VEN+AZA arm based on the number of patients with at least one post- treatment value. VENCLEXTA in Combination with Azacitidine or Decitabine The safety of VENCLEXTA in combination with azacitidine (N=67) or decitabine (N=13) was evaluated in M14-358, a non-randomized trial of patients with newly diagnosed AML. At baseline, patients were ≥75 years of age, or had comorbidities that precluded the use of intensive induction chemotherapy based on at least one of the following criteria: baseline ECOG performance status of 2-3, severe cardiac or pulmonary comorbidity, moderate hepatic impairment, CLcr <45 mL/min, or other comorbidity [see Clinical Studies (14.2)]. Patients received VENCLEXTA 400 mg orally once daily after completion of the ramp-up phase in combination with azacitidine (75 mg/m2 either intravenously or subcutaneously on Days 1-7 of each 28-day cycle) or decitabine (20 mg/m2 intravenously on Days 1-5 of each 28-day cycle). Azacitidine The median duration of exposure to VENCLEXTA when administered in combination with azacitidine was 6.5 months (range: 0.1 to 38.1 months). The safety of VENCLEXTA in combination with azacitidine in this trial is consistent with that of VIALE-A. Decitabine The median duration of exposure to VENCLEXTA when administered in combination with decitabine was 8.4 months (range: 0.5 to 39 months). Serious adverse reactions were reported in 85% of patients who received VENCLEXTA with decitabine, the most frequent (≥10%) being sepsis (excluding fungal; 46%), febrile neutropenia (38%), and pneumonia (31%). One (8%) fatal adverse reaction of bacteremia occurred within 30 days of starting treatment. Permanent discontinuation of VENCLEXTA due to adverse reactions occurred in 38% of patients. The most frequent adverse reaction leading to permanent discontinuation (≥5%) was pneumonia (8%). Dosage reductions of VENCLEXTA due to adverse reactions occurred in 15% of patients. The most frequent adverse reaction leading to dose reduction (≥5%) was neutropenia (15%). Dosage interruptions of VENCLEXTA due to adverse reactions occurred in 69% of patients. The most frequent adverse reactions leading to dose interruption (≥ 10%) were neutropenia (38%), febrile neutropenia (23%), leukopenia (15%), and pneumonia (15%). The most common adverse reactions (≥30%) were febrile neutropenia (69%), fatigue (62%), constipation (62%), musculoskeletal pain (54%), dizziness (54%), nausea (54%), abdominal pain (46%), diarrhea (46%), pneumonia (46%), sepsis (excluding fungal; 46%), cough (38%), pyrexia (31%), hypotension (31%), oropharyngeal pain (31%), edema (31%), and vomiting (31%). The most common laboratory abnormalities (≥30%) were neutrophils decreased (100%), lymphocytes decreased (100%), white blood cells decreased (100%), platelets decreased (92%), calcium decreased (85%), hemoglobin decreased (69%), glucose increased (69%), magnesium decreased (54%), potassium decreased (46%), bilirubin increased (46%), albumin decreased (38%), alkaline phosphatase increased (38%), sodium decreased (38%), ALT increased (31%), creatinine increased (31%), and potassium increased (31%). VENCLEXTA in Combination with Low-Dose Cytarabine VIALE-C The safety of VENCLEXTA in combination with low-dose cytarabine (VEN+LDAC) (N=142) versus placebo with low-dose cytarabine (PBO+LDAC) (N=68) was evaluated in VIALE-C, a double-blind randomized trial in patients with newly diagnosed AML. At baseline, patients were ≥75 years of age, or had comorbidities that precluded the use of intensive induction chemotherapy based on at least one of the following criteria: baseline ECOG performance status of 2-3, severe cardiac or pulmonary comorbidity, moderate hepatic impairment, CLcr <45 mL/min, or other comorbidity [see Clinical Studies (14.2)]. Patients were randomized to receive VENCLEXTA 600 mg orally once daily after completion of a 4-day ramp-up phase in combination with low-dose cytarabine (20 mg/m2 subcutaneously once daily on Days 1-10 of each 28-day cycle) or placebo in combination with low-dose cytarabine. Among patients who received VEN+LDAC, the median duration of exposure to VENCLEXTA was 3.9 months (range: <0.1 to 17.1 months). Serious adverse reactions were reported in 65% of patients who received VEN+LDAC, with the most frequent (≥10%) being pneumonia (17%), febrile neutropenia (16%), and sepsis (excluding fungal; 12%). Fatal adverse reactions occurred in 23% of patients who received VEN+LDAC, with the most frequent (≥5%) being pneumonia (6%) and sepsis (excluding fungal; 7%). Adverse reactions led to permanent discontinuation of VENCLEXTA in 25% of patients, dose reductions in 9%, and dose interruptions in 63%. The most frequent adverse reaction (>2%) which resulted in permanent discontinuation of VENCLEXTA was pneumonia (6%). Adverse reactions which required a dose reduction in ≥1% of patients were pneumonia (1%) and thrombocytopenia (1%), and the adverse reactions which required a dose interruption in ≥5% of patients included neutropenia (20%), thrombocytopenia (15%), pneumonia (8%), febrile neutropenia (6%), and sepsis (excluding fungal; 6%). Among patients who achieved bone marrow clearance of leukemia, 32% underwent dose interruptions for ANC <500/microliter. Table 17 presents adverse reactions identified in VIALE-C. Table 17. Adverse Reactions (≥10%) in Patients with AML Who Received VEN+LDAC with a Difference Between Arms of ≥5% for All Grades or ≥2% for Grade 3 or 4 Compared with PBO+LDAC in VIALE-C VENCLEXTA + Low-Dose Placebo + Low-Dose Cytarabine Cytarabine Adverse Reaction (N = 142) (N = 68) All Grades Grade 3 or 4 All Grades Grade 3 or 4 (%) (%) (%) (%) Gastrointestinal disorders Nausea 42 1 31 0 Diarrhea 28 3 16 0 Vomiting 25 <1 13 0 a Abdominal pain 15 <1 9 3 b Stomatitis 15 1 6 0 Blood and lymphatic system disorders Febrile neutropenia 32 32 29 29 Infections and infestations Pneumoniac 29 19 21 21 Vascular Disorders Hemorrhaged 27 8 16 1 e Hypotension 11 5 4 1 Musculoskeletal and connective tissue disorders VENCLEXTA + Low-Dose Placebo + Low-Dose Cytarabine Cytarabine Adverse Reaction (N = 142) (N = 68) All Grades Grade 3 or 4 All Grades Grade 3 or 4 (%) (%) (%) (%) f Musculoskeletal pain 23 3 18 0 General Disorders and Administration Site Conditions Fatigueg 22 2 21 0 Nervous System Disorders Headache 11 0 6 0 a Includes abdominal pain, abdominal pain upper, abdominal discomfort, and abdominal pain lower. b Includes stomatitis, mouth ulceration, aphthous ulcer, glossitis, mucosal inflammation, and tongue ulceration. c Includes pneumonia, lung infection, lower respiratory tract infection, pneumonia fungal, lower respiratory tract infection fungal, pneumocystis jirovecii pneumonia, pneumonia aspiration, pneumonia cytomegaloviral, and pneumonia pseudomonal. d Includes epistaxis, conjunctival hemorrhage, hemoptysis, gastrointestinal hemorrhage, gingival bleeding, mouth hemorrhage, upper gastrointestinal hemorrhage, hematuria, retinal hemorrhage, catheter site hemorrhage, cerebral hemorrhage, gastric hemorrhage, gastritis hemorrhagic, hemorrhage intracranial, hemorrhage subcutaneous, lip hemorrhage, mucosal hemorrhage, pharyngeal hemorrhage, post procedural hemorrhage, pulmonary alveolar hemorrhage, pulmonary hemorrhage, tooth pulp hemorrhage, uterine hemorrhage, and vascular access site hemorrhage. e Includes hypotension and orthostatic hypotension. f Includes back pain, arthralgia, pain in extremity, musculoskeletal pain, myalgia, neck pain, non-cardiac chest pain, arthritis, bone pain, musculoskeletal chest pain, and spinal pain. g Includes fatigue and asthenia. Other clinically important adverse reactions (All Grades) at ≥10% that did not meet criteria for Table 17 or <10% are presented below: Hepatobiliary disorders: cholecystitis/cholelithiasisa (1%) Infections and infestations: sepsisb (excluding fungal; 15%), urinary tract infectionc (8%) Metabolism and nutrition disorders: decreased appetite (19%), tumor lysis syndrome (6%) Nervous system disorders: dizzinessd (9%) Respiratory, thoracic, and mediastinal disorders: dyspneae (10%) Investigations: weight decreased (9%). a Includes cholecystitis and cholecystitis acute b Includes sepsis, bacteremia, septic shock, neutropenic sepsis, staphylococcal bacteremia, streptococcal bacteremia, bacterial sepsis, Escherichia bacteremia, pseudomonal bacteremia, and staphylococcal sepsis c Includes urinary tract infection and escherichia urinary tract infection d Includes dizziness and vertigo e Includes dyspnea and dyspnea exertional. Table 18 describes laboratory abnormalities identified in VIALE-C. Table 18. New or Worsening Laboratory Abnormalities (≥10%) in Patients with AML Who Received VEN+LDAC with Difference Between Arms of ≥5% for All Grades or ≥ 2% for Grade 3 or 4 Reactions Compared with PBO+LDAC in VIALE-C VENCLEXTA + Low-Dose Placebo + Low-Dose Cytarabine Cytarabine Laboratory Abnormality All Grades Grade 3 or 4 All Grades Grade 3 or 4 (%) (%) (%) (%) Hematology Platelets decreased 97 95 92 90 Neutrophils decreased 95 92 82 71 Lymphocytes decreased 92 69 65 24 Hemoglobin decreased 63 57 57 54 Chemistry Bilirubin increased 61 7 38 7 Albumin decreased 61 6 43 4 Potassium decreased 56 16 42 14 Calcium decreased 53 8 45 13 Glucose increased 52 13 59 9 AST increased 36 6 37 1 Alkaline phosphatase increased 34 1 26 1 ALT increased 30 4 26 1 Sodium increased 11 3 6 1 The denominator used to calculate the rate varied from 38 to 68 in the PBO+LDAC arm and from 65 to 142 in the VEN+LDAC arm based on the number of patients with at least one post- treatment value. M14-387 The safety of VENCLEXTA in combination with low-dose cytarabine (N=61) was evaluated in M14-387, a non-randomized, open- label trial of patients with newly diagnosed AML [see Clinical Studies (14.2)]. At baseline, patients were ≥75 years of age, or had comorbidities that precluded the use of intensive induction chemotherapy based on at least one of the following criteria: baseline ECOG performance status of 2-3, severe cardiac or pulmonary comorbidity, moderate hepatic impairment, CLcr <45 mL/min, or other comorbidity. Patients received VENCLEXTA 600 mg orally once daily after completion of the ramp-up phase in combination with low-dose cytarabine (20mg/m2 subcutaneously on Days 1-10 of each 28-day cycle). The safety of VENCLEXTA in combination with low-dose cytarabine is consistent with that of VIALE-C. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorization of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form https://sideeffects.health.gov.il

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים האלה:1 .בשילוב עם Obinutuzumab לטיפול בלוקמיה מסוג CLL בחולה שטרם קיבל טיפול סיסטמי למחלתו.משך הטיפול בתכשיר להתוויה זו לא יעלה על שנה.הטיפול לא יינתן בשילוב עם Ibrutinib.2. לוקמיה מסוג CLL בחולה שמחלתו חזרה (relapsed) לאחר או הייתה עמידה (refractory) לטיפול קודם. הטיפול יינתן כמונותרפיה או בשילוב עם Rituximab. הטיפול לא יינתן בשילוב עם Ibrutinib.הטיפול בתרופה יינתן לחולה שטרם טופל ב-Venetoclax למחלתו. 3. לוקמיה מסוג AML בחולה שטרם קיבל טיפול סיסטמי למחלתו ואינו מתאים לטיפול בכימותרפיה אינטנסיבית. הטיפול יינתן בשילוב עם Cytarabine במינון נמוך (LDAC) או בשילוב עם תרופות ממשפחת ה-Hypomethylating agents (HMAs) – Azacitidine או Decitabine. ב. מתן התרופה האמורה ייעשה לפי מרשם של מומחה באונקולוגיה או מומחה בהמטולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| טיפול בלוקמיה מסוג CLL - חולים עם מחלה עמידה או רפרקטורית ל-Ibrutinib, שאינם בעלי מוטציה מסוג del17p | ||||
| טיפול ב-CLL חוזרת בחולים עם מוטציה מסוג del 17p | ||||
| לוקמיה מסוג AML בחולה שטרם קיבל טיפול סיסטמי למחלתו ואינו מתאים לטיפול בכימותרפיה אינטנסיבית | ||||
| לוקמיה מסוג CLL בחולה שמחלתו חזרה (relapsed) לאחר או הייתה עמידה (refractory) לטיפול קודם |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
12/01/2017
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
17.04.18 - עלון לצרכן 26.03.17 - עלון לצרכן 27.03.17 - עלון לצרכן 28.08.17 - עלון לצרכן עברית 26.03.17 - עלון לצרכן 27.03.17 - עלון לצרכן 03.09.19 - עלון לצרכן 18.04.21 - עלון לצרכן אנגלית 02.05.22 - עלון לצרכן אנגלית 02.05.22 - עלון לצרכן עברית 18.04.21 - עלון לצרכן ערבית 02.05.22 - עלון לצרכן ערבית 16.03.23 - עלון לצרכן אנגלית 04.04.23 - עלון לצרכן עברית 16.03.23 - עלון לצרכן ערבית 31.01.24 - עלון לצרכן עברית 15.03.24 - עלון לצרכן אנגלית 15.03.24 - עלון לצרכן ערבית 11.04.19 - החמרה לעלון 03.09.19 - החמרה לעלון 26.04.20 - החמרה לעלון 04.06.20 - החמרה לעלון 04.06.20 - החמרה לעלון 18.08.20 - החמרה לעלון 12.01.21 - החמרה לעלון 29.03.21 - החמרה לעלון 13.04.21 - החמרה לעלון 27.02.22 - החמרה לעלון 02.05.22 - החמרה לעלון 04.04.23 - החמרה לעלון 01.02.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
ונקלקסטה 10 מ"ג טבליות