Quest for the right Drug
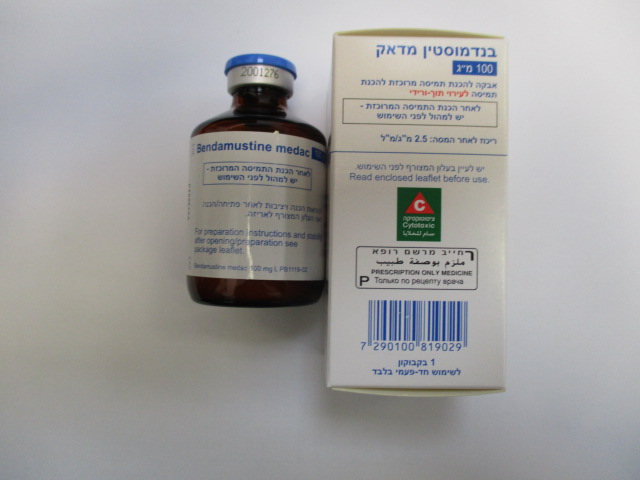
בנדמוסטין מדאק 100 מ"ג BENDAMUSTINE MEDAC 100 MG (BENDAMUSTINE HYDROCHLORIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
אבקה להכנת תמיסה מרוכזת לעירוי : POWDER FOR CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Antineoplastic agents, alkylating agents. ATC code: L01AA09 Bendamustine hydrochloride is an alkylating antitumour agent with unique activity. The antineoplastic and cytocidal effect of bendamustine hydrochloride is based essentially on a cross-linking of DNA single and double strands by alkylation. As a result, DNA matrix functions and DNA synthesis and repair are impaired. The antitumour effect of bendamustine hydrochloride has been demonstrated by several in-vitro studies in different human tumour cell lines (breast cancer, non-small cell and small cell lung cancer, ovarian carcinoma and different leukaemia) and in-vivo in different experimental tumour models with tumours of mouse, rat and human origin (melanoma, breast cancer, sarcoma, lymphoma, leukaemia and small cell lung cancer). Bendamustine hydrochloride showed an activity profile in human tumour cell lines different to that of other alkylating agents. The active substance revealed no or very low cross-resistance in human tumour cell lines with different resistance mechanisms at least in part due to a comparatively persistent DNA interaction. Additionally, it was shown in clinical studies that there is no complete cross- resistance of bendamustine with anthracyclines, alkylating agents or rituximab. However, the number of assessed patients is small. Chronic lymphocytic leukaemia The indication for use in chronic lymphocytic leukaemia is supported by a single open label study comparing bendamustine with chlorambucil. In the prospective, multi-centre, randomised study, 319 previously untreated patients with chronic lymphocytic leukaemia stage Binet B or C requiring therapy were included. The first line therapy with bendamustine hydrochloride 100 mg/m² i.v. on days 1 and 2 (BEN) was compared to treatment with chlorambucil 0.8 mg/kg days 1 and 15 (CLB) for 6 cycles in both arms. Patients received allopurinol in order to prevent tumour lysis syndrome. Patients with BEN have a significantly longer median progression free survival than patients with CLB treatment (21.5 versus 8.3 months, p < 0.0001 in the latest follow-up). Overall survival was not statistically significantly different (median not reached). The median duration of remission was 19 months with BEN and 6 months with CLB treatment (p < 0.0001). The safety evaluation in both treatment arms did not reveal any unexpected undesirable effects in nature and frequency. The dose of BEN was reduced in 34% of the patients. Treatment with BEN was discontinued in 3.9% of patients due to allergic reactions. Indolent non-Hodgkin's lymphomas The indication for indolent non-Hodgkin's lymphomas relied on two uncontrolled phase II trials. In the pivotal prospective, multi-centre, open study 100 patients with indolent B-cell non-Hodgkin´s lymphomas refractory to rituximab mono- or combination therapy were treated with BEN single agent. Patients had received a median of 3 previous chemotherapy or biological therapy courses. The median number of previous rituximab-containing courses was 2. The patients had had no response or there had been progression within 6 months after rituximab treatment. The dose of BEN was 120 mg/m² i.v. on days 1 and 2 planned for at least 6 cycles. Duration of treatment depended on response (6 cycles planned). The overall response rate was 75% including 17% complete (CR and CRu) and 58% partial response as assessed by independent review committee. The median duration of remission was 40 weeks. BEN was generally well tolerated when given in this dose and schedule. The indication is further supported by another prospective, multi-centre, open study including 77 patients. The patient population was more heterogeneous including indolent or transformed B-cell non- Hodgkin's lymphomas refractory to rituximab mono- or combination therapy. The patients had no response or there had been progression within 6 months or had had an untoward reaction to prior rituximab treatment. Patients had received a median of 3 previous chemotherapy or biological therapy courses. The median number of previous rituximab-containing courses had been 2. The overall response rate was 76% with a median duration of response of 5 months (29 [95% CI 22.1, 43.1] weeks). Clinical studies in patients with non-Hodgkin’s lymphoma in combination with rituximab: The pivotal randomized phase III study compared the first-line treatment of 4-week cycles of bendamustine hydrochloride 90 mg/m² i.v. on days 1 and 2 in combination with 375 mg/m² rituximab i.v. on day 1 (BR therapy) with 3-week cycles of rituximab 375 mg/m² i.v. on day 1 and standard-CHOP (750 mg/m2 cyclophosphamide, 50 mg/m2 doxorubicin, 1.4 mg/m2 vincristine and 100 mg prednisone) in 549 patients with advanced indolent non-Hodgkin’s lymphoma (NHL) and mantle cell lymphoma. In 82% of BR patients and 86% of R-CHOP patients the maximal of 6 cycles were administered. A statistically significant and clinical relevant improvement of progression free survival according to investigator assessment was observed for BR patients as compared to R-CHOP patients (median 61.4 months vs. 31.3 months, HR=0.607, p<0.0001). With the exception of the comparable results of marginal-zone lymphoma this significant difference of the progression free survival between the two treatments remained also in the histological sub-entities and age groups (<65 years and ≥65 years). The BR treatment also resulted in significantly higher complete response rates (43% vs. 29%, p<0.0009). After assessment by the independent review committee the progression free survival according to WHO criteria was 23.3 vs 30.6 months, HR=0.735 (0.5, 1.08), p=0.0420) and according to IWG criteria 33.1 vs. 28.2 months, HR=0.687 (0.45, 1.05), p=0.03. The interim analysis of the independent review committee of a further randomized, open parallel group study with bendamustine hydrochloride and rituximab (BR) compared to rituximab, cyclophosphamide, vincristine and prednisone (R-CVP) or rituximab. Cyclophosphamide, doxorubicin, vincristine and prednisone (R-CHOP) in the first line treatment of 336 patients with advanced indolent NHL or mantle-cell lymphoma showed a better response in favour of BR (complete remissions 31% vs. 25%; overall response 96% vs. 91%), too. The response in the indolent NHL population was of equal dimension. Myellosuppression (72% vs. 43%), alopecia (35% vs. 3%) as well as neuropathia (25% vs. 3%) were more common during R-CHOP/R-CVP treatment, whereas in the BR treatment arm more skin and hypersensitivity reactions were observed (16% vs. 8% and 10% vs. 4%).
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Distribution The elimination half-life t1/2ß after 30 min i.v. infusion of 120 mg/m2 area to 12 subjects was 28.2 minutes. Following 30 min i.v. infusion the central volume of distribution was 19.3 l. Under steady-state conditions following i.v. bolus injection the volume of distribution was 15.8-20.5 l. More than 95% of the substance is bound to plasma proteins (primarily albumin). Biotransformation A major route of clearance of bendamustine is the hydrolysis to monohydroxy- and dihydroxy- bendamustine. Formation of N-desmethyl-bendamustine and gamma-hydroxy-bendamustine by hepatic metabolism involves cytochrome P450 (CYP) 1A2 isoenzyme. Another major route of bendamustine metabolism involves conjugation with glutathione. In-vitro bendamustine does not inhibit CYP 1A4, CYP 2C9/10, CYP 2D6, CYP 2E1 or CYP 3A4. Elimination The mean total clearance after 30 min i.v. infusion of 120 mg/m2 body surface area to 12 subjects was 639.4 ml/minute. About 20% of the administered dose was recovered in urine within 24 hours. Amounts excreted in urine were in the order monohydroxy-bendamustine> bendamustine> dihydroxy- bendamustine> oxidised metabolite> N-desmethyl bendamustine. In the bile, primarily polar metabolites are eliminated. Hepatic impairment In patients with 30 - 70% tumour infestation of the liver and mild hepatic impairment (serum bilirubin < 1.2 mg/dl) the pharmacokinetic behaviour was not changed. There was no significant difference to patients with normal liver and kidney function with respect to Cmax, tmax, AUC, t1/2ß, volume of distribution and clearance. AUC and total body clearance of bendamustine correlate inversely with serum bilirubin. Renal impairment In patients with creatinine clearance > 10 ml/min including dialysis dependent patients, no significant difference to patients with normal liver and kidney function was observed with respect to Cmax, tmax, AUC, t1/2ß, volume of distribution and clearance. Elderly subjects Subjects up to 84 years of age were included in pharmacokinetic studies. Higher age does not influence the pharmacokinetics of bendamustine.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
